Medicare Advantage Inpatient Claim "Shadow Billing" - JE Part A
Medicare Advantage Inpatient Claim "Shadow Billing"
CMS requires hospitals and skilled nursing facilities (SNFs) to submit claims to the A/B MACs or Fiscal Intermediaries (FI) and to the Medicare Advantage (MA) plans for inpatient services provided to Medicare beneficiaries who are enrolled in an MA plan.
Note: Because MA plan cards do not utilize an identical informational format, be sure to copy both the Medicare and the MA plan card when the patient is admitted.
Hospitals
Inpatient Prospective Payment System (PPS) hospitals, Inpatient Rehabilitation Facilities (IRFs), and Long-Term Care Hospitals (LTCHs) must submit two claims for inpatient stays by Medicare Advantage beneficiaries. Sometimes called "shadow billing," these claims must be filed with both the MA and the A/B MAC or FI so that the inpatient days to be captured and included in the disproportionate share and low-income patient (LIP) calculations. The information also is used for computation of the hospital’s Indirect Medical Education payment.
If a hospital meets the disproportionate share hospital definition, an additional operating cost payment will be made for discharges. The LIP adjustment accounts for differences in costs among IRFs associated in the proportion of low-income patients treated. Additional information about the calculations can be found in CMS Change Request (CR) 5647.
The claims should be submitted as covered, and should include the following:
- Type of bill 11X
- Condition code 04 (information only bill)
- Condition code 69 (teaching hospitals only - code indicates a request for a supplemental payment for Indirect Medical Education/Graduate Medical Education/Nursing and Allied Health)
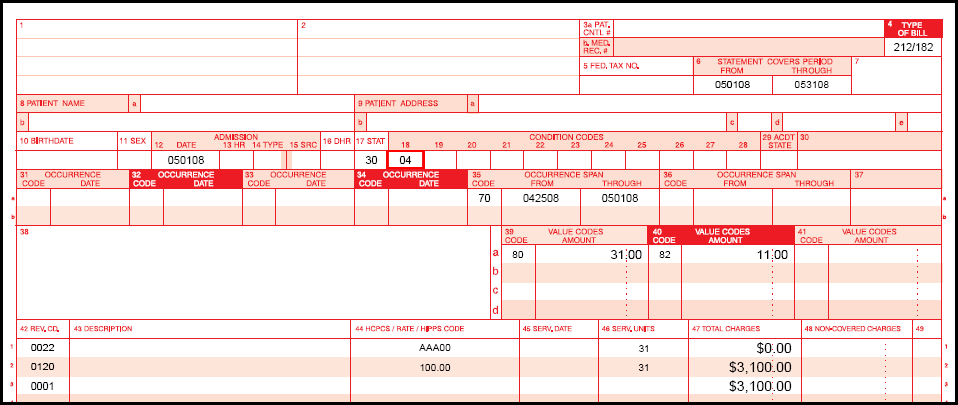
PPS, IRF, and LTCH UB-04 Example
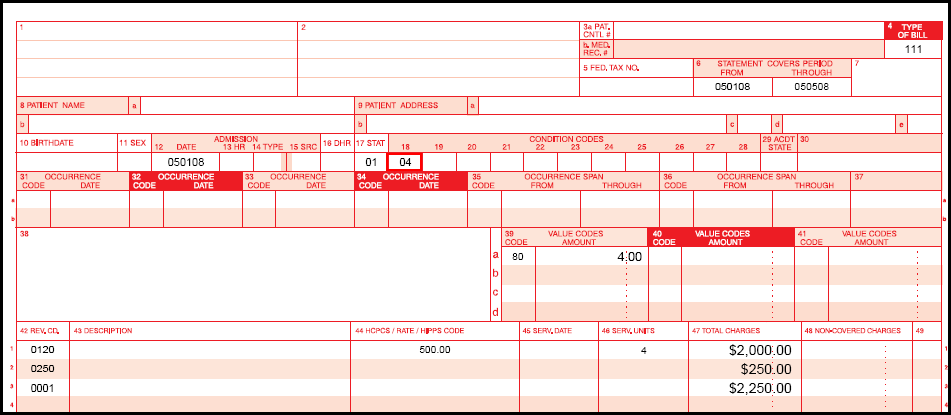
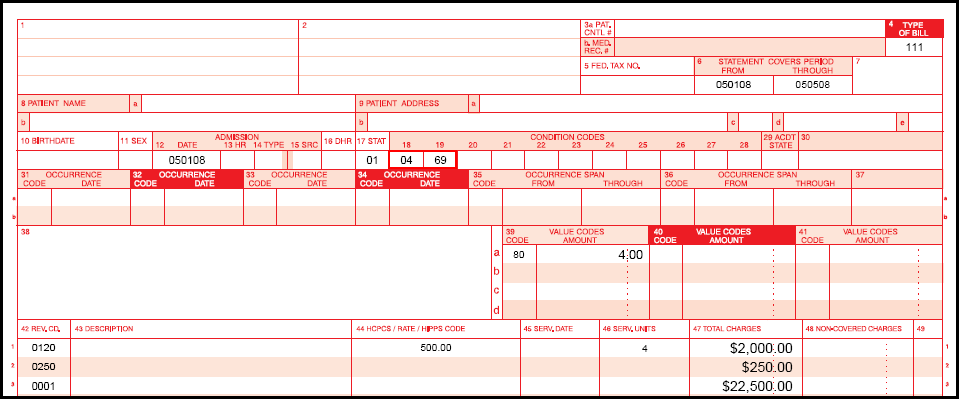
Teaching Hospital UB-04 Example
Skilled Nursing Facilities/Swing Bed Units
To maintain correct benefit period information, SNFs and swing bed units must submit claims to the AB MAC/FI in addition to the claims they submit to the MA plans so long as the beneficiary remains at a skilled level of care. The coding used on these claims will allow the AB MAC/FI to override edits requiring prior qualifying stay data so the skilled days can be added to the Common Working File.
The claims should be submitted as covered, and should include the following:
- Type of Bill 21X or 18X
- Condition Code 04
The condition code will indicate that the claim is being submitted for information only, and the FI/MAC will not issue payment in addition to the amount paid by the MA plan.
SNF/Swing Bed UB-04 Example