Credit Balance Report - Details Page Completion - JE Part A
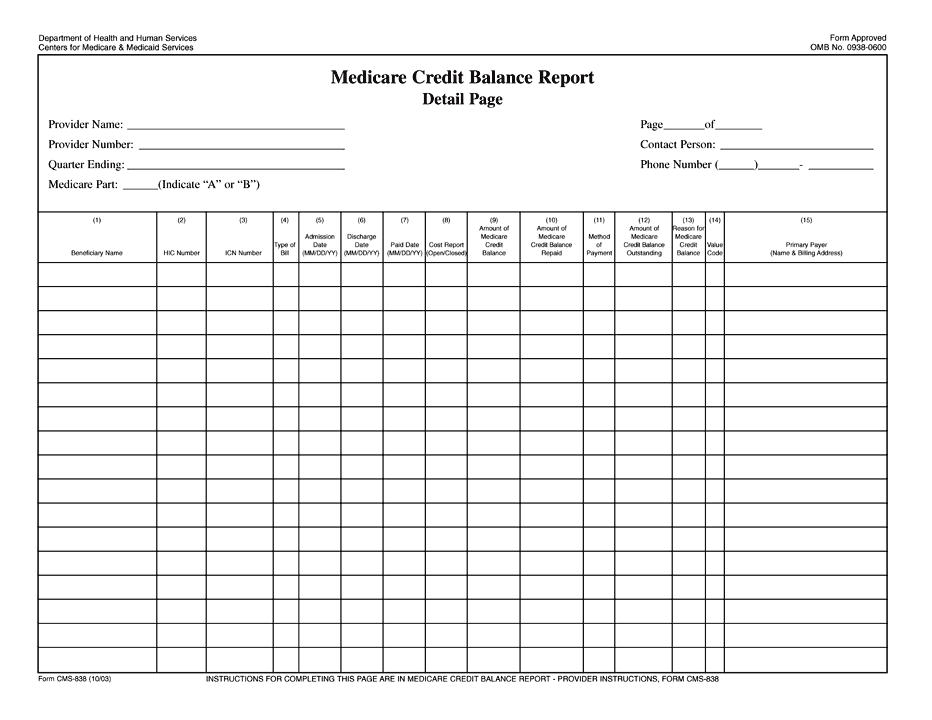
Credit Balance Report - Details Page Completion
Within 30 days of each quarter, Providers must complete two pages of the Credit Balance Report, the Certification Page and a Detail Page for each provider or subunit.
Move your cursor over any of the fields or check boxes below to view a pop-up explaining how to complete each area of the Details Page of the Credit Balance Report.
Last Updated $dateUtil.getDate( $modifieddate , "MMM dd , yyyy" , $locale , $tzone )
