Medically Unlikely Edit (MUE) - JD DME
MUE Lookup Tool
Medically Unlikely Edit (MUE)
The Centers for Medicare & Medicaid Services (CMS) developed Medically Unlikely Edits (MUEs) to reduce the paid claims error rate for Part B claims. An MUE for a HCPCS/CPT code is the maximum units of service a provider would order under most circumstances for a single beneficiary on a single date of service. Not all HCPCS codes have an MUE. The Medically Unlikely Edit (MUE) Lookup Tool on this page, provides guidance for published MUEs for DME HCPCS codes. Although CMS publishes most MUE values on its website, other MUE values are confidential and are for CMS and CMS contractors' use only. The latter group of MUE values is not published.
Questions/Concerns
You may submit inquiries about the National Correct Coding Initiative (NCCI) program, including those related to NCCI (PTP, MUE, and Add-on Code) edits, in writing via email to NCCIPTPMUE@cms.hhs.gov.
Any submissions made to the NCCI program that contain Personally Identifiable Information (PII) or Protected Health Information (PHI) are automatically discarded, regardless of the content.
Inquiries about a specific claim or how to submit an appeal should be addressed to the Medicare Administrative Contractor (MAC).
For MUE frequently asked questions and answers (FAQs), MUE files, and the Publication Announcement Letter, which explain most aspects of the MUE program, see the CMS Medically Unlikely Edits webpage.
MUE Adjudication Indicator (MAI)
Describes the type of MUE Adjudication Indicator (MAI) claim line or date of service. For date of service (DOS) indicators, a narrative may be required for an explanation, as permitted by the policy. i.e., specific supply duration (60-day or 90-day) or different strengths (J codes) etc.
Indicator MAI 1
Indicates a value adjudicated by claims processing systems at the claim line level. Appropriate use of modifiers to report the same HCPCS code on separate lines of a claim will enable the reporting of medically necessary units of service in excess of MUE utilizing the GA modifier.
- Example: The same HCPCS code is provided and billed on multiple claim lines (overutilization) with different modifiers. One modifier may be GA, indicating a valid ABN was obtained.
Indicator MAI 2
Indicates an absolute date of service edit based on policy, such as anatomical considerations, the definition of the code, or published CMS policy. CMS has not identified any instances in which a higher value than the one displayed is payable. For DOS MUEs, the claims processing system sums all units of service (UOS) on all claim lines with the same HCPCS code and DOS based on a three-month supply maximum, as permitted by the policy.
When billing the same HCPCS code with identical modifiers, all UOS must be consolidated on one claim line with a narrative indicating valid justification. i.e., the specific supply duration (60-day or 90-day) or different strengths (J codes, etc.) that necessitate the inclusion of a narrative for explanation. This measure is necessary to process claims correctly without encountering denials, providing smoother and more efficient claim processing related to policy frequency limits, as stated in the Standard Documentation Requirements under claim narratives.
- Example: There are no valid reasons to receive payment for a greater value than displayed in the MUE tool, regardless of supporting documentation.
- On a single DOS, the supplier can provide up to a three-month supply, as permitted by the policy.
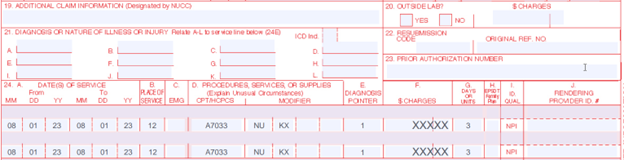
Incorrect Billing Example
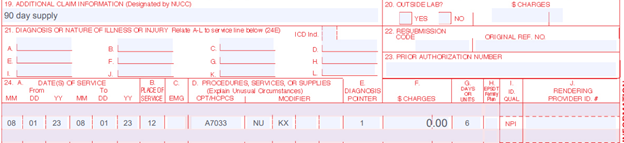
Correct Billing Example with a Narrative, including valid justification i.e., the specific supply duration (60-day or 90-day) or different strengths (J codes) etc., in Item 19 of the 1500 hard copy claim form or the 2400/NTE segment of an electronic claim.
Indicator MAI 3
Indicates a value adjudicated by claims processing systems at the date of service level. If claim denials based on these edits are appealed, MACs may pay UOS in excess of the MUE value if there is adequate documentation of medical necessity of correctly reported units. For DOS MUEs, the claims processing system sums all UOS on all claim lines with the same HCPCS code and DOS. These are "per-day edits based on clinical benchmarks."
- Example: It is unlikely for a supplier to provide the same value or more that displays in the MUE tool on a correctly coded claim. A claim with this value or more will be denied as an excessive/unnecessary number of UOS in the typical delivery of such items to beneficiaries. Suppliers should be prepared with sufficient supporting documentation that identifies why the beneficiary needed the displayed value, or more UOS on the same day and same side to appeal the claim.
