Disproportionate Share Hospital (DSH) - JE Part A
Disproportionate Share Hospital (DSH)
Access the below related information from this webpage.
- Background
- Eligibility
- Medicaid Days
- Section 1115 Waiver Days
- Baby Days
- Out of State Days
- California Providers
- Documentation
- Resources
Background
The Medicaid program was established as part of the Social Security Amendments of 1965. It was designed to provide health coverage for low-income individuals and families. In the early years of Medicaid, it became evident that some hospitals were serving a significantly higher number of low-income and uninsured patients, leading to financial strains. To address the financial burden faced by hospitals serving a disproportionate number of Medicaid and uninsured patients, Congress established the DSH program as part of the Omnibus Budget Reconciliation Act of 1981 (OBRA '81). The DSH program aimed to provide additional federal funds to qualifying hospitals based on specific criteria. These criteria included the percentage of Medicaid and low-income patients served and the hospital's Medicare utilization rate. Over the years, the DSH program went through several expansions and revisions to adapt to changing healthcare needs and regulations. These changes included adjustments to the DSH formula and funding mechanisms. The DSH program operates as a partnership between the federal government and individual states. Federal funding is provided to states, which then distribute it to eligible DSH hospitals within their jurisdiction.
The Affordable Care Act (ACA), signed into law in 2010, made several changes to the DSH program. It aimed to reduce DSH payments over time, assuming that with Medicaid expansion and decreased uninsured rates, the need for such payments would decrease. Some states chose to expand Medicaid under the ACA, increasing the number of people with access to Medicaid coverage. This had an impact on the DSH program by reducing the number of uninsured patients and changing the landscape for DSH-eligible hospitals. The DSH program continues to evolve, facing challenges related to healthcare policy changes, budget constraints, and the ongoing debate over Medicaid expansion.
Eligibility
To be eligible for Medicare DSH payments, hospitals must meet specific criteria regarding the proportion of low-income and Medicaid patients they serve. These criteria are defined by federal regulations and can vary depending on the hospital's location and other factors.
Hospitals must also comply with reporting requirements and regulations. Compliance ensures that hospitals accurately represent their patient population and financial needs.
The first method of eligibility is commonly referred to as the "Pickle Method". Under this method, the hospital must be located in an urban area and have 100 or more beds. The hospital's location, whether classified as urban or rural, is determined in accordance with the definitions in 42 CFR 412.62, except in the case that a reclassification results from an urban hospital is reclassified as rural as set forth in 42 CFR 412.103. If the hospital can prove that during the Cost Reporting period, more than 30% of its net inpatient care revenues come from State and local government payments for care given to patients with low incomes. If these requirements are met, the hospital may receive a DSH adjustment.
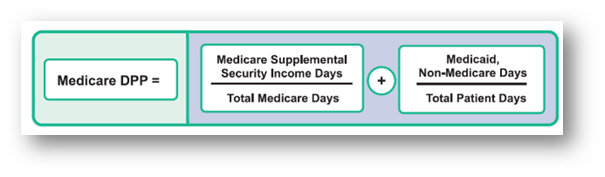
The second method is the most common way of qualifying for the DSH payment adjustment. This method is based upon a complex statutory formula under which DSH payment adjustments are based on the hospital's geographic designation, the number of beds in the hospital, and the level of the hospital's Disproportionate Patient Percentage, or DPP. DPP is the sum of two fractions: the Medicare Fraction and the Medicaid Fraction. The Medicare Fraction is calculated by dividing the number of the hospital's inpatient days furnished to patients who were entitled to both the Medicare Part A and Supplemental Security Income, or SSI, benefits by the hospital's total number of patient days furnished to patients entitled to benefits under Medicare Part A. The Medicaid fraction is calculated by dividing the hospital's number of inpatient days furnished to patients who, on those days, were eligible for Medicaid, but were not eligible to benefits under Medicare Part A, by the hospital's total number of inpatient days in the same period.
Medicaid Days
When calculating the number of Medicaid days, the hospital must determine if the patient was eligible for Medicaid under a State plan approved under Title XIX on the same day of service. For this, allowable medical assistance is limited to an approved Title XIX State Plan, not medical assistance under a State-only program or other program. For the purpose of Medicare DSH calculation, Medicaid days refers to days on which the patient is eligible for medical assistance benefits under an approved Title XIX State Plan. This includes days in which Medicaid did not make payment for any services.
Excluded Days
General Assistance Patient Days - Patients that are covered under a State-only or County-only general assistance program are not Medicaid-eligible under the State plan, regardless of whether or not any payment is available for health care services under the program
Unverifiable State Days - Days in which patients cannot be verified by State records have fallen within a period wherein the patient was eligible for Medicaid
Days in Excluded Units - Days in the Psychiatric, Skilled Nursing, or Rehabilitation Units of PPS hospitals. PPS Rehab units should still submit separate listings and report the days separately on the Cost Report. Some states paid claims listings fail to separately identify the Title XIX excluded unit days but have the capability to do so. The hospital bears the burden of proof; therefore it is the hospital's responsibility to have the State identify the days and remove them from eligible Title XIX days
Dual Entitlement Days - Those who are entitled to both Medicare Part A and Medicaid on that day. These dual-eligible patients are included in the Medicare fraction, but not the Medicaid fraction as indicated in 69 Fed. Ref. 49048. Even if a patient has exhausted Medicare Part A coverage for inpatient hospital services they remain entitled to other Part A benefits and it therefore would still count as a dual entitlement day. Once eligibility has been determined for the patient for Medicaid under a State plan approved under Title XIX, the hospital must determine if any days are dual entitlement days. In the case that there are dual entitlement days, those days must be subtracted from the Medicaid fraction in the calculation.
Section 1115 Waiver Days
Section 1115 of the Social Security Act gives the Secretary authority to allow XIX funding in ways not otherwise allowed. This "waives" some regular Medicaid rules. It also grants states flexibility for innovative projects that align with the objectives of the state Medicaid program. These waivers are generally approved for an initial 5-year period and can be extended for additional periods. Section 1115 waivers have been used to: expand populations and benefits not otherwise covered under a State Plan, impose cost-sharing and make provider payments not permitted under a State Plan, change delivery systems, invest in healthcare infrastructure, responses to public health emergencies, and restrict benefits/populations otherwise covered under a State Plan.
Upon request, providers shall be able to supply documentation for a selected sample that ensure they accurately included the inpatient stay in the Section 1115 waiver program for reimbursement through the funding pool based on the provider's Section 1115 approved program documents and have accurately included the inpatient stay on the Section 1115 log.
Baby Days
Each state has their own eligibility rules for baby days. Most states say the baby's eligibility follows the mother's eligibility for a period of time, such as 30 or 60 days. Providers will need to check with their state to determine their state's policy on baby days for DSH eligibility.
Out of State Days
Out of State Days are allowable DSH days and can be claimed and submitted on a separate list. Hospitals will need to obtain verification of Title XIX eligibility from each state other than their own, and that the patient is not eligible for Medicare. Payment support (Medicaid Remittance Advice) is NOT sufficient proof. Hospitals will need to have the State DSH Eligibility Report that shows the patient was eligible for medical assistance benefits under an approved Title XIX State Plan during the dates of services.
California Providers
Types of Medi-Cal DSH days:
- Code 1 Days - days that are fully eligible for Title XIX funding
- Documentation: UB04(9) or itemized bill, copy of patient face sheet/admission form, patient account history, State Title 19 eligibility verification file
- Code 2 or 3 Restricted Eligibility Days - these are days that are eligible for Title XIX funding only in specific situations
- Documentation: UB04(9) or itemized bill, copy of patient face sheet/admission form, patient account history, State Title 19 eligibility verification file, Medi-Cal paid claim detail report, Treatment Authorization Request (TAR), Emergency Report and Doctors' Notes
- Code 4 Days - these are not allowable DSH days - they relate to patients that the State Eligibility verification system cannot find in their Eligibility database
Eligibility vs. Restricted Eligibility
- Eligibility: the patient is eligible for full scope benefits without any limitation
- A patient who is fully eligible does not have any Restricted Aid Code because that patient is not subject to any "restriction". These are Code 1 days
- Restricted Eligibility: the patient is covered, not for the full scope benefits or medical services in general, but is "restricted" to certain medical services. They will have Restricted Aid Codes, or RAC, that restrict or limit the services for which they will be covered by Medi-Cal. There are two types of RAC:
- RAC codes which are State-only Codes, or Codes for patient services that are funded solely by funds from the State of CA
- RAC which are Codes for patient services that are paid in part by the state of CA and in part by Federal funds or Title XIX funds
- For DSH days to be claimed for reimbursement, the provider should only include patient days covered by codes that have Title XIX funds (Codes 2 & 3 DSH days)
- In California, the only type of inpatient services that have Title XIX matching funding for Restricted Eligible patients is for emergency and/or pregnancy related services
Baby Days
- A baby's eligibility follows the mother's eligibility on the month of birth and the subsequent month. After that the baby should have their own eligibility.
- Hospitals should perform an eligibility verification transaction before rendering services to the infant. Eligibility of children born to mothers covered by Medicaid at the date of the child's birth must be supported by:
- UB for the mother and the baby
- Support for the mother's Medi-Cal eligibility
- Upon notification of the birth of a child to a mother who was eligible only for Medicaid coverage of labor and delivery as emergency medical services, pursuant to section 1903(v) of the Social Security Act, the State shall immediately issue a separate identification number for the child.
Documentation
Required documentation that should be submitted to allow Medicaid days to be included in the DSH calculation includes:
- State DSH Eligibility Verification Report with the listing of days claimed
- A log(s) listing the patient names and dates of service which shows the total Medical Assistance, or MA, and MA eligible days claimed in the Medicaid fraction
- The State Eligibility Verification Report, which will detail if patients are dual-eligible or not
- The patient's UB-92 or UB-04 or other financial/medical history must be made available to the auditor to ensure that days are not being claimed for services that were incurred in excluded units
- If a hospital submits an amended cost report, then they must also submit either an amended listing or addendum to the original listing of the hospital's Medicare Eligible Days that corresponds to the Medicaid Eligible Days being claimed in the amended cost report.
It is important providers save their documentation for each fiscal year in the case of a reopening request. Without the proper documentation to support, our auditors will not be able to verify information.
If you have any questions regarding DSH or DSH Medicaid Eligible Days, call the Noridian Provider Contact Center.
