How to Read an ADR - JE Part B
How to Read an ADR
An Additional Documentation Request (ADR) is a request sent to the provider by Mail outlining a specific service or code under review. Information below will assist how to read an ADR letter that encompasses more than one Date of Service on the same claim. The same information will apply to multiple lines of the same Code and same Date of Service billed on the same claim.
Here is an example of a multi-day ADR letter. There will be multiple pages sent with the same ADR letter for each code or service on the claim to be reviewed.
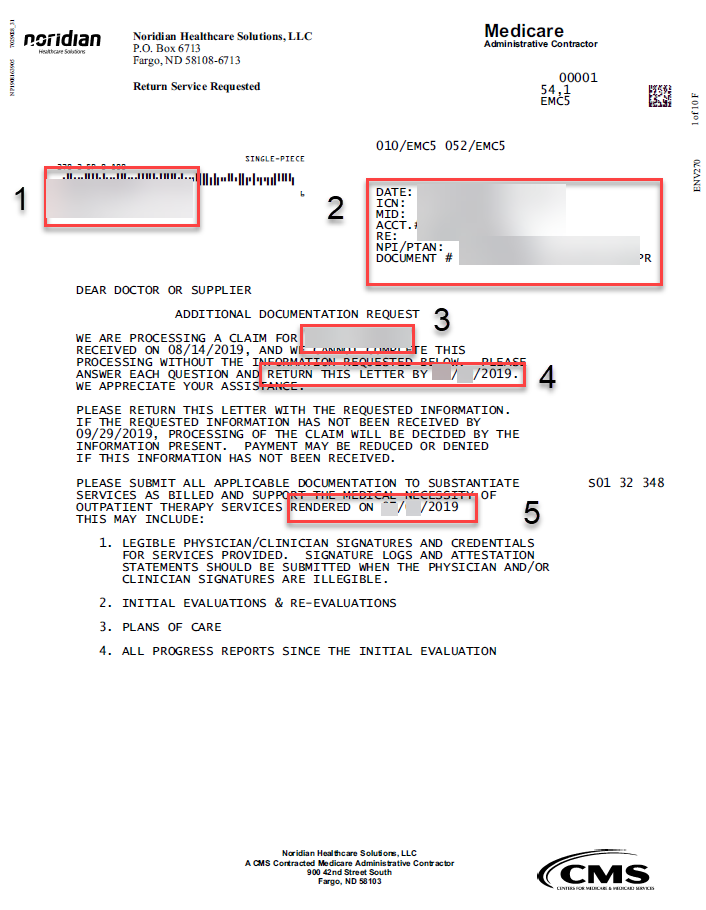
The first portion of the letter is the first code under claim review. Each subsequent code under review will follow.
- Provider's address on file. This is where all documentation relating the the Review will be sent.
- Date, ICN, MID, RE:, NPI/PTAN, Document number
- Date: This is the date the claim was developed by the system. The provider will have 45 days from this date to submit documentation.
- ICN: 13 Digit MCS Claim number
- MID: Partially obscured Patient ID Number
- Acct #: Provider submitted Account number. This number is not Noridian or System generated, it will only have significance to the Provider/Facility.
- RE: Beneficiary's Name
- NPI/PTAN: Rendering Provider's NPI
- Document #: Full document number. May be referenced by provider if ICN or XREF (cross reference) is not available.
- Beneficiary's name on the Claim.
- Date documentation needs to be submitted by. This is 45 days after the Date shown under number 2.
- Date of Service on the claim for the first code under review.
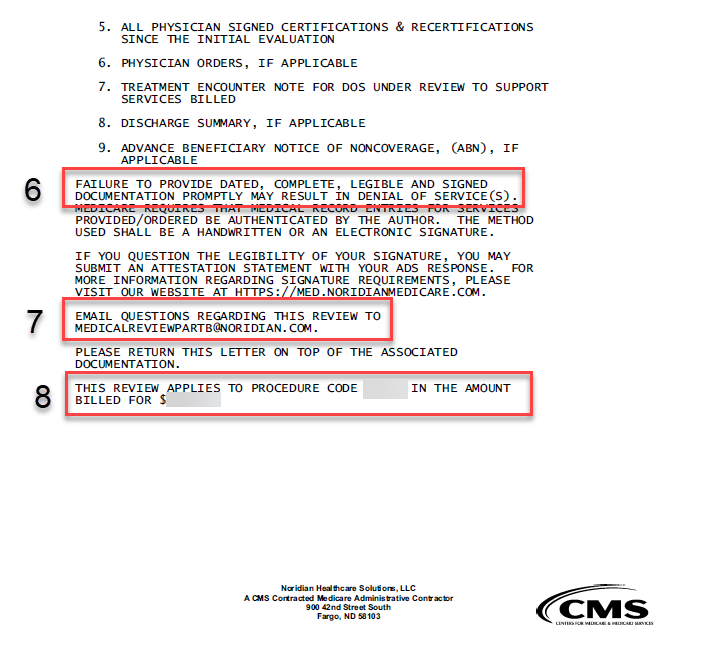
- Notice stating that services will be denied if documentation is not received within 45 days.
- Email address for Medical Review Part B. Use this address to ask any questions relating to your Review.
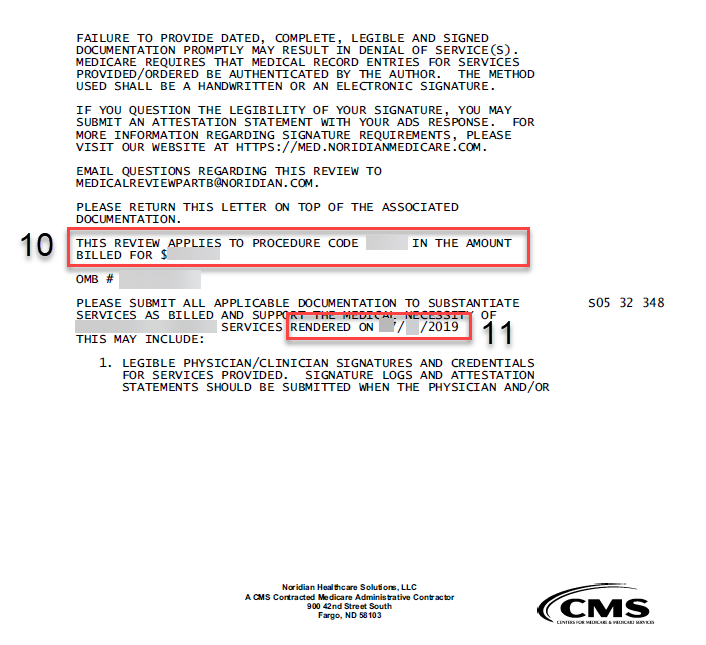
- Lists the actual CPT or HCPC Code under review and the dollar amount the code was billed for on the claim.
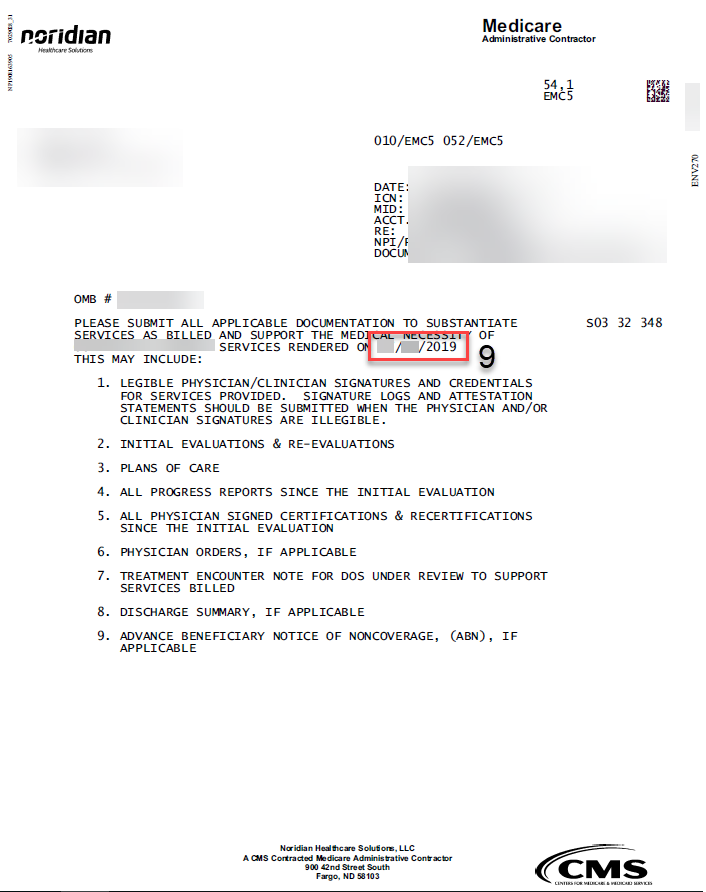
- Second date of service billed on the claim with a code that is being reviewed.
- Listing of second CPT or HCPC Code under review and the dollar amount the code was billed for.
- In repeating fashion: Date of Service for the third code on the claim under review, and so on.
