ABN Tutorial - JF Part B
Advance Beneficiary Notice of Noncoverage (ABN) Form Tutorial
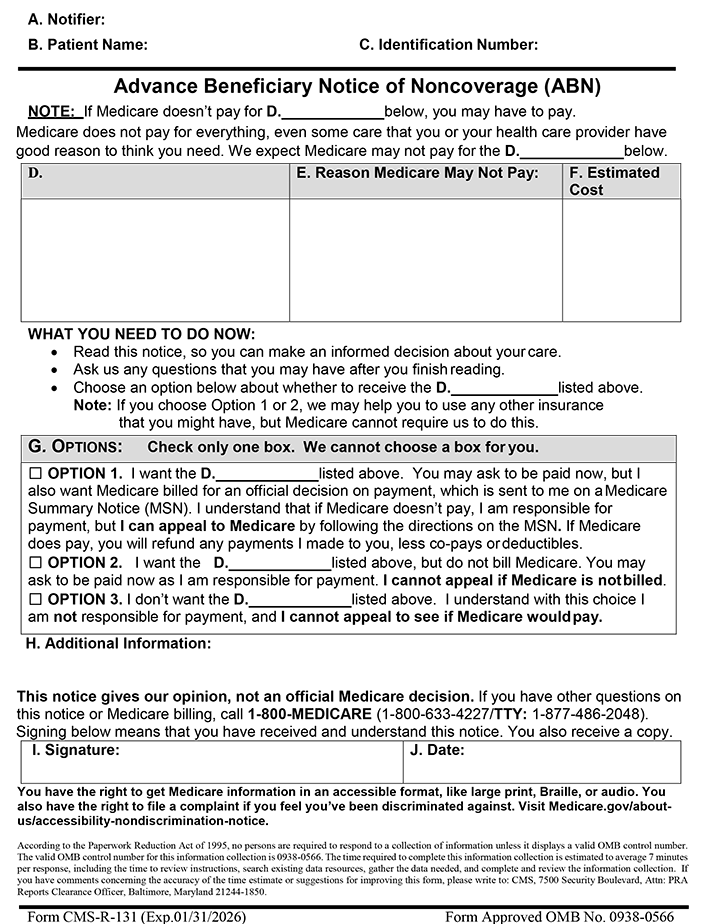
For more information on how to complete the ABN form, move your cursor over any field in the interactive form below; you'll see instructions on how to complete the field. You may also click in any field for more detailed instructions.