Hemophilia Clotting Factor Billing - JF Part B
Hemophilia Clotting Factor Billing
Medicare Part B covers administration of blood clotting factors and related items used for hemophilia patients able to use such factors without medical supervision. Hemophilia encompasses the following conditions:
- Factor VIII deficiency (classic hemophilia); hemophilia A-J7185, J7186, J7190, J7192);
- Factor IX deficiency (hemophilia B, plasma thromboplastin component (PTC) or Christmas factor deficiency (J7193, J7194, J7195, J7200-J7203); and
- Von Willebrand's disease (J7192)
- Additional HCPCS: J7170, J7175, J7179-J7183, J7187-J7189, J7198, J7204-J7205, J7207-J7213
- 2023 HCPCS:
- J7177 (Injection, human fibrinogen concentrate (fibryga), 1 mg )
- J7178 (Injection, human fibrinogen concentrate, not otherwise specified, 1 mg)
- J7214 (Injection, factor viii/von willebrand factor complex, recombinant {altuviiio}, per factor viii i.u.)
Part B blood clotting factors are priced as a drug and biological under the drug pricing fee schedule. A furnishing fee will be paid for items and services associated with the clotting factor.
2025 Clotting Factors: Alhemo and Qfitlia
Medicare Part B now pays for Alhemo (concizumab-mtci) and Qfitlia (fitusiran) as FDA approved clotting factors and eligible for the furnishing fee. Bill with Not Otherwise Code, since HCPCS are not assigned as of this posting.
- Alhemo - December 20, 2024: routine prophylaxis to prevent or reduce the frequency of bleeding episodes in adult and pediatric patients 12 years of age and older with hemophilia A (congenital factor VIII deficiency) with factor VIII inhibitors or hemophilia B (congenital factor IX deficiency) with factor IX inhibitors.
- Qfitlia - March 28, 2025: routine prophylaxis to prevent or reduce the frequency of bleeding episodes in adult and pediatric patients 12 years of age and older with hemophilia A or B, with or without factor VIII or IX inhibitors.
Note: The electronic claim examples below are for PC-ACE users. Providers not using PC-ACE should contact their software vendor for claim completion assistance.
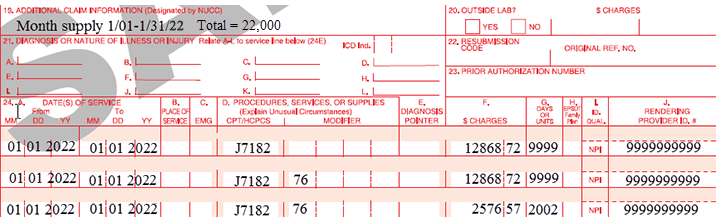
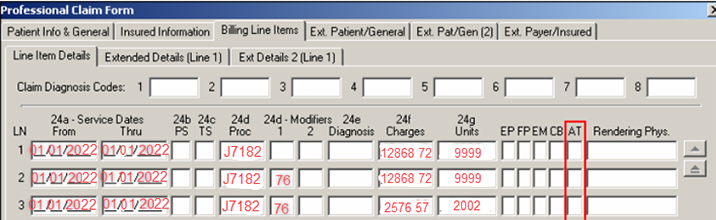
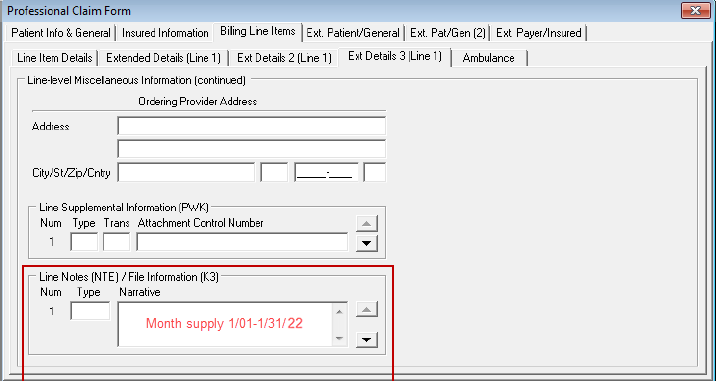
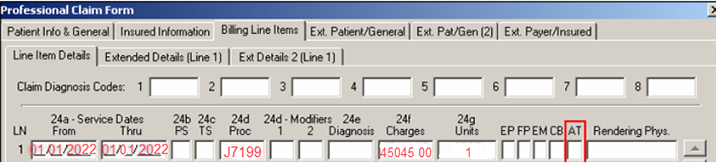
Billing Instructions for MUEs Over 9,999 Units Per Claim
Due to claims processing system limitations, if the total MUEs exceed 9,999 per claim, divide claim lines up to the allowable MUEs per claim line (9,999). For example, J7182 has a per line MUE of 22,000. Due to the system limitations, each claim line is split up to the 9,999 MUE limitation; with excess billed on a third line (2002).
Do not span the dates on the claim line, but enter the date span in the narrative with total units (22,000). Append modifier 76 to any second and subsequent lines.
CMS-1500 Claim Example
Electronic Claim Example
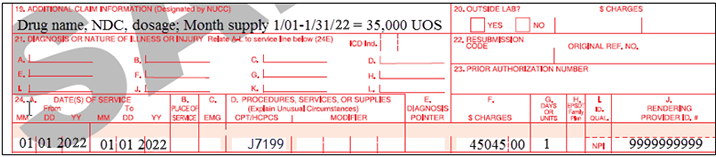
Billing Instructions for Not Otherwise Classified Codes
For Not Otherwise Classified HCPCS codes (NOC), enter the drug name, dosage and NDC in Loop 2400, SV101-7 segment (preferred) or Loop 2400, NTE02 for electronic claims. Loop 2400, segment SV104 (quantity billed) must be entered as "one" (1). Paper claim submitters must enter the number of units per line in Item 19 of the CMS-1500 claim form and the quantity billed as "one" (1).
CMS-1500 Claim Example
Electronic Claim Example
Dollar Amount Exceeds $99,999.99
If providing a month supply and the total billed amount exceeds $99,999.99, two claims must be submitted.
Additional Important Claim Information
- If required information is not submitted, claims will be denied as unprocessable. When codes are denied as unprocessable, provider must correct claim error and resubmit it
- If claim denies due to number of units exceeds acceptable maximum (for example N362), verify MUEs and number of allowable units. MUEs denied have appeal rights. Medical documentation must support services rendered
Date of Service
If the Factor VIII is administered within a facility or "incident to" a physician service, the actual date the drug was administered should be used as the DOS. If the Factor VIII is billed by a pharmacy, to replenish the patient's home supply, the date of delivery must be the DOS billed.
Documentation
The amount of clotting factors determined to be necessary to have on hand and thus covered under this provision will be based on the historical utilization pattern or profile developed by the carrier for each patient. Changes in a patient's medical needs over a period of time may require adjustments in the profile. It is expected that the treating source, e.g., a family physician or Comprehensive Hemophilia Diagnostic and Treatment Center, will have such information.
For hemophilia factors, we would expect:
- The diagnosis on a claim must be one of the hemophilia diagnosis codes
- Provider's prescription must include:
- Name of drug
- Concentration (if applicable)
- Dosage to include initiation date, frequency of administration, duration of infusion (if applicable), signature, date and any other individual state requirements
- Record from the physician's office must include evidence of medical necessity
- Copy of this medical record must be provided on request
Resource
- CMS Internet Only Manual (IOM), Publication 100-02, Medicare Benefit Policy Manual, Chapter 6, Section 30
- CMS IOM Publication 100-02, Medicare Benefit Policy Manual, Chapter 15, Section 50-50.6
- CMS IOM Publication 100-03, National Coverage Determination (NCD) Manual, Chapter 1, Part 2, Section 110.3
- CMS IOM Publication, 100-04, Medicare Claims Processing Manual, Chapter 3, Section 20.7.3
- CMS IOM Publication 100-04, Medicare Claims Processing Manual, Chapter 17, Section 80.4
