Appealing Demand Letters - JF Part B
Appealing Demand Letters
When Medicare (Noridian) or other outside contract Comprehensive Error Rate Testing (CERT), Recover Auditor, or the Supplemental Medical Review Contractor (SMRC) has determined that an overpayment has occurred, a Demand Letter is issued. Providers are given 30 days from the date of the Demand Letter to pay the requested overpayment amount. To avoid interest from accruing, timely payment is necessary.
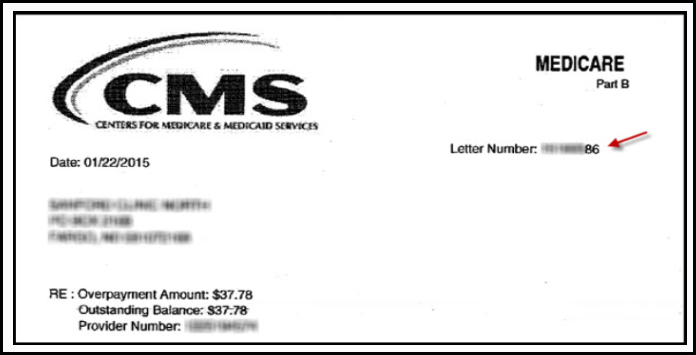
The Demand Letter includes detailed information necessary to satisfy the overpayment and information on how to submit an appeal if there is a disagreement with the overpayment. The Demand Letter will also be assigned a Letter Number which is used to identify what has been demanded by Medicare.
Demand Letter Example
If a provider disagrees with the overpayment decision, an appeal may be filed. An appeal is an independent review separate from the review of the initial determination. The first level of an appeal is a redetermination. A redetermination request must be filed within 120 days from the date of the Demand Letter. However, to avoid recoupment from occurring, the redetermination must be filed within 30 days from the date of the demand letter. Unless otherwise shown, Noridian will assume the demand letter was received by the provider within five days from the date on the letter.
The following items must be submitted when appealing Demand Letters.
- Overpayment Invoice
- Entire copy of the Demand Letter
- Completed Redetermination Request Form - Signature Required Form. Complete all form fields. An incomplete request is counted as a dismissal, view the Redetermination/Reopening Form Tutorial for completion assistance.
- Appeal Request for Multiple Beneficiaries: Do not submit in a spreadsheet format. To be sure that nothing is missed in the review process, the contractor requests that each date of service for each beneficiary be submitted separately with the Redetermination Request form and supporting documentation.
- Medical Documentation support medical necessity
- Appointed Representative(s) who are appealing on behalf of the provider or beneficiary must include a completed Appointment of Representative (AOR) form
Request Options
Electronic Submission
- Submit via Noridian Medicare Portal (NMP). It's fast, secure and economical
- Access educational resources, learn how to register, and view user manual on NMP webpage
Fax Submission
- Fax appeal requests to General Inquiries fax number available on Fax Numbers webpage
- To ensure submitted faxes are received by Noridian and processed in a timely manner, follow below guidelines
- Direct fax to correct Noridian department
- Submit a fax cover sheet which includes:
- Total number of pages
- Noridian department name
- Provider name
- Provider contact information
- Submit a single fax transmission with all documents to support a single claim/request
- There is not a system in place to consolidate multiple fax receipts to a single claim, inquiry, appeal etc.
- Submit a separate fax for each claim, inquiry, or response with all supporting documentation attached for that specific claim
- Review clarity of documents being faxed to ensure contents will not be distorted when faxed
- Highlights, shading, previously faxed pages where legibility may be further diminished if re-faxed
Paper Submission
- Send Redetermination request to Overpayment Redetermination Request address on Mailing Addresses webpage
Resource
Overpayments and Next Steps
When an overpayment has occurred, a Demand Letter is issued. When a demand letter is received, providers have the following options:
Agree with the Overpayment:
- Send Noridian a check for the owed money
- Request an Immediate Offset
Disagree with the Overpayment
- Submit a Rebuttal if the overpayment action will cause financial hardship (A rebuttal will not stop the recoupment activities)
- Submit a Redetermination Request

